Flourish Founder Megan Nivens-Tannett had her first brush with mortality at a very young age when she learned that her grandmother was dying of breast cancer at 54. It was devastating to watch, but she was so young and never really understood the reason for her early death until later in life. Growing up, the word ‘cancer’ seemed to pepper conversations focused on her family’s health and never seemed to escape the family dialogue. Fueled by her mother’s sage advice on proactive healthcare, Megan committed to preventative measures. At 35, she breathed a sigh of relief when genetic tests revealed she was BRCA-negative, dodging what many consider the “ticking time bomb” in women’s health.

4 Generations of Megan’s family.
Flash forward to 2023: While Megan was waiting to be seen for her annual OBGYN appointment, a never-seen-before Nurse treated her and expressed a heightened interest when it came time to review her family history. The Nurse was intrigued, raised her eyebrows, and asked many questions, which took Megan by surprise. She saw her doctor yearly – and there’s never been such a heightened interest in her family history – until now. The Nurse eventually suggested that she take another genetic test, as advancements had come a long way since 2015. The results returned with unwanted information: Megan tested positive for a newly discovered breast cancer marker, the BARD1 mutation. Associated with the BRCA1 gene, the BARD1 gene typically helps prevent cancers, but the mutation increases the lifetime risk of breast cancer by as much as 40 percent. It’s a sobering turn of events, but Megan knows her story isn’t written yet. She has the information, and now she has the power to make informed choices for her future. And in doing so, she aims to rewrite her family’s troubled history with cancer once and for all.
As women, we’re expected to do it all, balancing career, family, and home while appearing calm and put together on the surface. When family members get sick, women traditionally take on the role of caretakers, even if they’re also unwell. This expectation of quiet strength, acceptance, and resilience often comes with the side effect of women getting the short end of the stick when it comes to being heard and respected at both the personal and professional levels.
Whether it’s mental or physical, recent or long term, women’s health concerns are too often ignored, with healthcare providers telling them that the symptoms they’re reporting are imaginary or just routine complaints that will go away on their own.
Women’s health can also be compared to that of the iceberg analogy – the small symptoms that appear on the surface can indicate much bigger underlying issues. A male patient may be able to walk into a doctor’s office and quickly get the diagnosis and treatment he needs, but for women, this can be a much lengthier and more difficult and frustrating process.
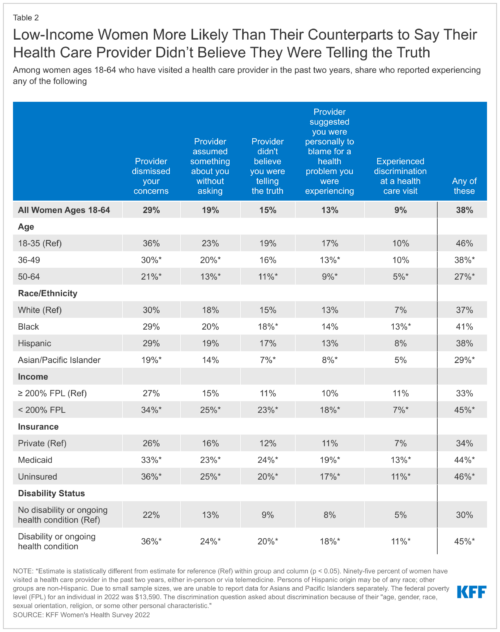
According to findings from KFF’s Women’s Health Care survey, 36% of women ages 18-35 reported that a healthcare provider dismissed their concerns, compared to 30% of women ages 36-49 and 21% of women ages 50-64. There was a similar trend with providers assuming something without the patients asking, not believing that the patients were telling the truth, and suggesting the patient was personally to blame for their health problems. While this applied to all women, it especially applied to younger women, women of color, and low-income patients.
Silent Killers
Things get more complicated when considering mental or physical health conditions that hide below the surface.
For instance, heart disease is commonly called the “Silent Killer.” While it’s a major cause of death for both men and women, the indicators are more commonly overlooked in women. That’s a big deal, because heart disease is a primary cause of death in women over 65. The CDC notes that despite heart disease being the leading cause of death for women in the United States, causing 1 in every 5 female deaths, research has shown that only about 56% of US women recognize that heart disease is their number 1 killer.
Medical professionals believed for a long time that women were at a lower risk for cardiovascular disease because of their higher estrogen levels. This belief was based largely on historical research that, for the most part, excluded women and especially women of color. In 2016, however, a report found a significant link between endometriosis and increased risk of coronary heart disease, finding that women with endometriosis are 62 percent more likely to have a heart attack, develop chest pain, or need heart procedures to open blocked arteries. In addition, women who experience gestational diabetes and high blood pressure during pregnancy also have an elevated risk of developing heart disease.
What you need to know about heart disease symptoms
In the movies, heart attacks are obvious, with victims (usually male) suddenly grabbing their left arm or chest before collapsing. It’s generally much more subtle in real life, especially for women. That’s why it’s so important to know the signs and be aware of changes in your body. According to the CDC, some women have no symptoms, but others may experience the following either when resting or active:
- Angina–usually a dull or heavy feeling of discomfort or ache in the chest
- Pain in the neck, jaw, or throat
- Pain in the upper abdomen or back
- Nausea
- Vomiting
- Persistent and/or excessive tiredness
High blood pressure (hypertension) is a major risk factor for heart disease: Over 56 million women in the U.S., including almost 1 in 5 women of reproductive age, have high blood pressure (≥130/80 mm HG) or are taking blood pressure medicine.
Despite the risk, it’s often underdiagnosed in women, with fewer than 1 in 4 women with high blood pressure having it under control. Black women are nearly 60% more likely than White women to have high blood pressure, and pregnant women with high blood pressure have double the risk of developing heart disease later in life than pregnant women without this condition. In the United States, high blood pressure develops in 1 in every 8 pregnancies.
Some other underlying risk factors for heart disease include high LDL cholesterol, diabetes, stress, and depression. While these factors can impact women of any age, younger women are less likely to be routinely tested for them on the grounds that they’re associated with older patients.
Your body knows – do you?
Like heart disease, cancer is a health condition that requires intervention as soon as possible in order to prevent it from becoming a fatal disease. Because it’s so widely varied, it can be difficult to identify in its early stages, with many of the symptoms seeming to be minor irritations rather than signs of a life-threatening condition. In some cases, especially ovarian cancer, early stages can be asymptomatic or symptoms are mistaken for something common and less serious. It’s important to pay attention to unusual changes in your body and to discuss worrisome concerns with your doctor.
A few symptoms to be aware of:
- Persistent fatigue
- Unintended weight loss or gain
- Persistent, unexplained muscle or joint pain
- Skin changes, such as sores that won’t heal, changes to moles, and yellowing, darkening, or redness
- Digestive and urinary changes
- Persistent cough or trouble breathing
- Hoarseness
- Unexplained bleeding or bruising
- Lumps or thickening felt under skin
- Spotting after menopause
Autoimmune disorders are also frequently overlooked or misdiagnosed, especially in young women. If the symptoms aren’t readily visible, women often find themselves either putting up with them or struggling to find healthcare providers who will make a concerted effort to pin down the root cause. Getting a diagnosis is even more challenging when healthcare providers assume that the reported symptoms are exaggerated or not serious enough to warrant further investigation.
Knowing your family history is key – if one or both parents have a history of high cholesterol, diabetes, thyroid issues, cancer, or other health issues, there’s a good chance you will too. Going into a checkup with this knowledge allows you to present your healthcare provider with valid reasons to pay special attention to things they may not otherwise so they can be caught early. In our last installment, for instance, we noted that Dawn discovered that her thyroid wasn’t nearly as under control as she thought after her 26-year-old daughter’s discussion with her own doctor. Because she was aware of her family medical history, her daughter requested additional tests and learned that her cholesterol was also dangerously high despite being active and a healthy weight. The National Institute of Health (NIH) recommends screening every 5 years between ages 20 and 65, but she is now screened annually to ensure that her statins continue to keep her cholesterol under control.
“Just bad period pains:” Why reproductive health can’t be overlooked
For women of reproductive age, Polycystic Ovary Syndrome (PCOS) and endometriosis are commonly under- or misdiagnosed, causing not just debilitating pain but also a significant impact on daily life.
PCOS, linked to factors including hormonal imbalances and insulin resistance, affects around 5-10% of women of childbearing age, while endometriosis impacts 10-15% of women and is a progressive, painful condition characterized by the presence of endometrial (uterine) tissue growing outside of the uterus. Common symptoms are fertility issues, weight gain, and menstrual pain and irregularity. Endometriosis resolves with menopause, but the hormonal imbalance associated with PCOS continues to increase the risk of diabetes, stroke, and heart attack even after menopause.
According to a study of 4,334 women with endometriosis, 63% of patients were initially told nothing was wrong with them, with many women reporting that it took up to 10-12 years to get a diagnosis. The longer the wait, the more it can progress: over time, the pain can become more severe and even disabling, requiring surgery to remove the abnormal tissue growth.
Misdiagnosis is common with both, dismissed by doctors as nothing more than “bad period pains” or other health problems. PCOS can be detected through a physical exam to look for characteristic markers such as unusual hair growth or skin discoloration; pelvic exams and ultrasounds; and blood tests. Endometriosis, on the other hand, requires ultrasound, an MRI, and usually laparoscopic surgery to confirm a diagnosis. Multiple studies have found a significant hereditary link, with endometriosis passed down from both maternal and paternal family lines. Family histories and careful records of symptoms can speed the process of diagnosis, allowing you to walk into the doctor’s office armed with relevant information. There’s simply no reason to live your life in constant, debilitating pain if something can be done about it!
Getting the treatment you need can be challenging in a medical culture where women’s legitimate concerns might be brushed off as hypochondria, attention seeking, or exaggeration. It’s critical to ensure that your voice is heard and respected. Keeping a written log of persistent symptoms, including dates, times, and specific details can provide you with the evidence you need to help convince your doctor that additional testing is necessary. If they insist that it’s “just in your head” or something innocuous that will resolve on its own with a diet or a relaxing cup of chamomile tea, that’s your signal to find a new healthcare provider.
Mental Health Matters
Mental disorders impact both men and women, but women suffer differently from men. Women are also more likely to suffer in silence: one study notes that because women are more likely than men to feel stigmatized for seeking help with mental health issues, they’re less likely to get the treatment they need. The stigma is even greater among women of color: a report from Johns Hopkins University found that women are at least twice as likely to experience an episode of major depression as men, and compared to their Caucasian counterparts, Black women are only half as likely to seek help. That’s huge. According to Dr. Erica Richards, chair and medical director of the Department of Psychiatry and Behavioral Health at Sibley Memorial Hospital, there’s a common perception in a lot of Black communities that women have to be strong and stoic.
“Women are so busy taking care of everyone else – their partners, their elderly parents and their children – they don’t take care of themselves,” she said. “Women should be reminded that attending to their own needs, whether physical or emotional, doesn’t make you weak. It makes you better able to care for your loved ones in the long run.”
— Dr. Erica Richards
Postpartum Depression Can’t Be Ignored
Perinatal and postpartum depression are also a big deal: According to the World Health Organization, about 10% of pregnant women and 13% of women who have just given birth experience a mental disorder, primarily depression. It doesn’t just impair a woman’s ability to function, but it also hinders her children’s development.
According to the Mayo Clinic, most moms experience postpartum “baby blues” after childbirth, with common symptoms like mood swings, reduced concentration, irritability, and sadness beginning within the first few days after delivery and lasting for up to two weeks. However, a more intense and long-lasting form of depression, postpartum depression, can last for up to a year after birth and may interfere with a new mom’s ability to care for her baby, herself, and other daily tasks.
Postpartum depression is a serious problem that can impact every facet of life, with wide-ranging symptoms including anxiety and panic attacks, feelings of worthlessness, difficulty bonding with your baby, and even recurring thoughts of harming yourself or the baby. In rare cases, new moms can suffer from an even more extreme mood disorder called postpartum psychosis, which leads to severe symptoms including confusion and disorientation, obsessive thoughts about the baby, paranoia, and attempts to harm oneself or the baby.
As moms, we’re expected to do it all and because having a baby is supposed to be a joyous event, it may seem embarrassing or a sign of weakness to admit that you’re not okay. It’s important to remember that postpartum depression is not a character flaw or a weakness, but instead a complication of childbirth that needs to be understood so that it can be effectively treated with medicine and/or therapy. Women in the midst of it may not be able to recognize the signs or may be reluctant to admit needing help. It truly takes a village – if a friend or loved one doesn’t seem okay, reach out to let them know that help is available and that you’re looking out for them.
Gender matters with behavioral disorders
Boys are generally seen as being much more likely to have behavioral disorders such as ADD, ADHD, and Autism spectrum disorder (ASD). However, recent research indicates that the ratio between males and females with autism could be significantly lower than previously thought.
Researchers suggest that this is because symptoms manifest differently between girls and boys.
Once again, this goes back to the long-standing exclusion of female patients in medical research: because the symptoms experienced by female patients often differ from those commonly experienced by males, they are frequently overlooked or misdiagnosed.
According to a report from Durham University, women’s symptoms of autism and/or ADHD are often misdiagnosed or ignored, with female patients reporting being brushed off by healthcare providers, told they’re “not autistic” or that their problem is “anxiety and not ADHD.” Instead, they may be incorrectly diagnosed with other conditions such as Borderline Personality Disorder, eating disorders, bipolar disorder, and anxiety. Women may also learn over time to hide their symptoms from people, resulting in delayed diagnoses or misdiagnosis. In fact, as many as 80% of female patients remain undiagnosed by the age of 18, leading to missed early intervention. This can translate to significant social challenges, academic difficulty, behavioral issues, and a profound sense of being different from one’s peers.
Although diagnosis can raise fears of discrimination or that others will look down on them, it can also bring a sense of relief, empowerment, and a better quality of life.
There’s still a long way to go, but women’s health is starting to find its place in the spotlight thanks to a growing focus on including women and people of color in research and testing. The role of medical professionals in the advancement of women’s health is key, but they can’t do it alone – the power to drive change also comes from the patients themselves. Your healthcare is a collaborative effort, and you deserve to have a winning team on your side.
As we come to a close in our series for women’s health, we want to thank you for taking the time to read through something that has hit really close to home lately.
After a lot of discussion (and personal reflection), Megan decided to take back control of her health – once and for all. She’s proceeding with a double mastectomy + reconstructive surgery which will take place later this year. After all, she plans to have a lot of life yet to live – and we hope you do, too.